Resetting Expectations at Mediation: Fla. Stat. 768.0427 and Medical Damages in Florida
By: Raul Romaguera
Florida Supreme Court Certified Circuit Civil Mediator
Florida Supreme Court Qualified Arbitrator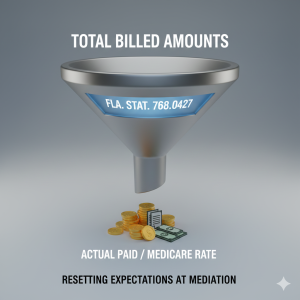
If the personal injury case you’re prosecuting or defending was filed after March 24, 2023, Fla.Sta. 768.0427 can be pivotal. It narrows the evidence juries may see, which in turn lowers the ceiling for settlement negotiations. Mediators and attorneys now frame discussions around actual paid amounts and disclosed LOPs, not inflated bills. This can result in a benefit to both sides when presented correctly at mediation or trial.
The statute provides as follows:
768.0427 Admissibility of evidence to prove medical expenses in personal injury or wrongful death actions; disclosure of letters of protection; recovery of past and future medical expenses damages.
***
(2) ADMISSIBLE EVIDENCE OF MEDICAL TREATMENT OR SERVICE EXPENSES. —Evidence offered to prove the amount of damages for past or future medical treatment or services in a personal injury or wrongful death action is admissible as provided in this subsection.
(a) Evidence offered to prove the amount of damages for past medical treatment or services that have been satisfied is limited to evidence of the amount actually paid, regardless of the source of payment.
(b) Evidence offered to prove the amount necessary to satisfy unpaid charges for incurred medical treatment or services shall include, but is not limited to, evidence as provided in this paragraph.
1. If the claimant has health care coverage other than Medicare or Medicaid, evidence of the amount which such health care coverage is obligated to pay the health care provider to satisfy the charges for the claimant’s incurred medical treatment or services, plus the claimant’s share of medical expenses under the insurance contract or regulation.
2. If the claimant has health care coverage but obtains treatment under a letter of protection or otherwise does not submit charges for any health care provider’s medical treatment or services to health care coverage, evidence of the amount the claimant’s health care coverage would pay the health care provider to satisfy the past unpaid medical charges under the insurance contract or regulation, plus the claimant’s share of medical expenses under the insurance contract or regulation, had the claimant obtained medical services or treatment pursuant to the health care coverage.
3. If the claimant does not have health care coverage or has health care coverage through Medicare or Medicaid, evidence of 120 percent of the Medicare reimbursement rate in effect on the date of the claimant’s incurred medical treatment or services, or, if there is no applicable Medicare rate for a service, 170 percent of the applicable state Medicaid rate.
4. If the claimant obtains medical treatment or services under a letter of protection and the health care provider subsequently transfers the right to receive payment under the letter of protection to a third party, evidence of the amount the third party paid or agreed to pay the health care provider in exchange for the right to receive payment pursuant to the letter of protection.
5. Any evidence of reasonable amounts billed to the claimant for medically necessary treatment or medically necessary services provided to the claimant.
(c) Evidence offered to prove the amount of damages for any future medical treatment or services the claimant will receive shall include, but is not limited to, evidence as provided in this paragraph.
1. If the claimant has health care coverage other than Medicare or Medicaid, or is eligible for any such health care coverage, evidence of the amount for which the future charges of health care providers could be satisfied if submitted to such health care coverage, plus the claimant’s share of medical expenses under the insurance contract or regulation.
2. If the claimant does not have health care coverage or has health care coverage through Medicare or Medicaid, or is eligible for such health care coverage, evidence of 120 percent of the Medicare reimbursement rate in effect at the time of trial for the medical treatment or services the claimant will receive, or, if there is no applicable Medicare rate for a service, 170 percent of the applicable state Medicaid rate.
3. Any evidence of reasonable future amounts to be billed to the claimant for medically necessary treatment or medically necessary services.
(d) This subsection does not impose an affirmative duty upon any party to seek a reduction in billed charges to which the party is not contractually entitled.
(e) Individual contracts between providers and authorized commercial insurers or authorized health maintenance organizations are not subject to discovery or disclosure and are not admissible into evidence.
(3) LETTERS OF PROTECTION; REQUIRED DISCLOSURES.—In a personal injury or wrongful death action, as a condition precedent to asserting any claim for medical expenses for treatment rendered under a letter of protection, the claimant must disclose:
(a) A copy of the letter of protection.
(b) All billings for the claimant’s medical expenses, which must be itemized and, to the extent applicable, coded according to:
1. For health care providers billing at the provider level, the American Medical Association’s Current Procedural Terminology (CPT), or the Healthcare Common Procedure Coding System (HCPCS), in effect on the date the services were rendered.
2. For health care providers billing at the facility level for expenses incurred in a clinical or outpatient setting, including when billing through an Ambulatory Payment Classification (APC) or Enhanced Ambulatory Patient Grouping (EAPG), the International Classification of Diseases (ICD) diagnosis code and, if applicable, the American Medical Association’s Current Procedural Terminology (CPT), in effect on the date the services were rendered.
3. For health care providers billing at the facility level for expenses incurred in an inpatient setting, including when billing through a Diagnosis Related Group (DRG), the International Classification of Diseases (ICD) diagnosis and procedure codes in effect on the date in which the claimant is discharged.
(c) If the health care provider sells the accounts receivable for the claimant’s medical expenses to a factoring company or other third party:
1. The name of the factoring company or other third party who purchased such accounts.
2. The dollar amount for which the factoring company or other third party purchased such accounts, including any discount provided below the invoice amount.
(d) Whether the claimant, at the time medical treatment was rendered, had health care coverage and, if so, the identity of such coverage.
(e) Whether the claimant was referred for treatment under a letter of protection and, if so, the identity of the person who made the referral. If the referral is made by the claimant’s attorney, disclosure of the referral is permitted, and evidence of such referral is admissible notwithstanding s. 90.502. Moreover, in such situation, the financial relationship between a law firm and a medical provider, including the number of referrals, frequency, and financial benefit obtained, is relevant to the issue of the bias of a testifying medical provider.
(4) DAMAGES RECOVERABLE FOR MEDICAL TREATMENT OR SERVICE EXPENSES.—The damages that may be recovered by a claimant in a personal injury or wrongful death action for the reasonable and necessary cost or value of medical care rendered may not include any amount in excess of the evidence of medical treatment and services expenses admitted pursuant to subsection (2), and also may not exceed the sum of the following:
(a) Amounts actually paid by or on behalf of the claimant to a health care provider who rendered medical treatment or services;
(b) Amounts necessary to satisfy charges for medical treatment or services that are due and owing but at the time of trial are not yet satisfied; and
(c) Amounts necessary to provide for any reasonable and necessary medical treatment or services the claimant will receive in the future
1. Defense Attorney Angles
* Anchor low with actual paid amounts: The jury won’t necessarily see the billed amounts; (This new law is at its infancy. Judges treat it differently.) they’ll only see the amount actually paid or 120% of the current Medicare reimbursement rate. That’s the real exposure to the defense, and it should guide settlement.
* Highlight transparency requirements: The plaintiff’s provider’s letter of protection and factoring agreements will be disclosed. That undermines inflated numbers and may weaken the plaintiff’s (and their attorney’s) credibility, thus strengthening the defense’s positions.
* Risk framing: Fla.Sta. 768.0427 caps what the jury can consider. Mediation might be your best chance to avoid a low verdict and get more now.
2. Plaintiff Attorney Angles
* Future damages emphasis: Even if past bills are limited, future care costs remain significant. The jury can still award for ongoing treatment.
* Settlement certainty: Fla. Sta. 768.0427 creates uncertainty. (This new law is at its infancy. Judges treat it differently.) Mediation lets us lock in a fair number without risking a low jury award.
* Emotional leverage: Regardless of billing rules, the human story of pain and suffering remains compelling; that value is preserved. Indeed, the value may be enhanced as Plaintiff’s counsel can focus in on plaintiff’s pain and suffering more with less dilution, distraction and forays into medical bills.
3. Mediation Conclusion
* Before Fla.Sta. 768.0427: Plaintiffs could leverage inflated medical bills to push settlements higher.
* After Fla. Sta. 768.0427: Defendants have stronger bargaining power, but plaintiffs can still argue future damages and non-economic losses.
* In mediation: The statute becomes the pivotal point; mediators use it to temper expectations and drive compromise. The plaintiff’s human pain and suffering is the real story, the medical bills become secondary. The defense will, of course, try to down play the pain and suffering and argue the economics. Any given jury may go either way and that’s the point of mediation in the first place.